Our Services
Temporomandibular
Joints (TMJ)
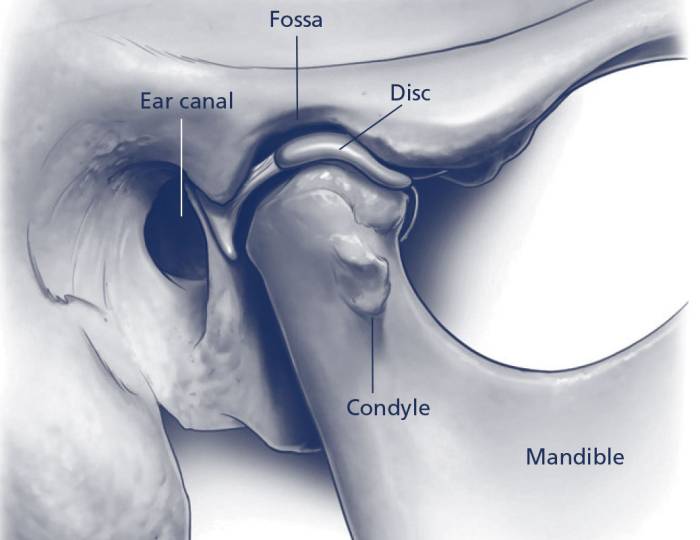
Located where the lower jaw attaches to the base of the skull, the temporomandibular joints (TMJs) allow the mouth to open and close, and move from side to side. When you place your fingers in front of your ears and open your mouth, you can feel these joints move. Muscles attached to the TMJ control its position and jaw movements during talking, chewing and swallowing.
A TMJ disorder can affect one or both TMJs, and can cause pain, locking, facial pain and headache. Although TMJ disorders are fairly common, of every 100 people with a TMJ disorder, only about five will need surgery. Non-surgical treatments can be very effective.
The cause of a TMJ disorder is not always known. Most symptoms are caused by joint degeneration or injury to the jaws. Chronic TMJ pain and dysfunction can be difficult to treat.
TMJ Surgical Procedures
The main reasons for surgery are that the TMJ disorder is not responding to non-surgical treatment and symptoms of chronic pain and dysfunction are interfering with the patient’s normal activities and enjoyment of life. The four types of surgical procedures to treat a TMJ disorder are:
Arthroscopy
A miniature telescope is inserted into the TMJ to see and treat any defects or pathology.
Arthrocentesis & lavage
The TMJ is washed out with a special solution to reduce inflammation and pain, and to improve jaw function.
Arthrotomy
This is open surgery of the TMJ that allows the surgeon to examine the joint, perform various corrective procedures to the joint, and biopsy tissue, if necessary.
Total Replacement
Similar to other joints, a TMJ may become dysfunctional to the point where it should be replaced with a prosthesis made of metal alloys and synthetics.
What you need to know
Your Medical History
Your surgeon needs to know your medical history to plan the best treatment for you. Tell your surgeon about ALL medicines that you take and other health problems you may have. Some may interfere with treatment, surgery, anaesthesia and recovery.
A Decision To Have A Surgery
As you make the decision whether to have non-surgical or surgical treatment, be sure that you understand the risks, benefits and limitations of the treatment options. Only you can decide if surgery is right for you. If you have any questions, ask your surgeon.
Anaesthesia
Surgical treatment of a TMJ may be performed under local anaesthesia, local anaesthesia with conscious sedation, or general anaesthesia. Your surgeon will explain more about the type of anaesthesia that is best in your case.

Possible Risks & Complications
Modern surgical techniques and prostheses have greatly improved the surgical outcomes.
However, there are risks of complications, as with all types of surgery. Risks of complications and additional information are more fully outlined in the complete ANZAOMS patient education pamphlet and should be discussed with your oral and maxillofacial surgeon.
Source: Australian and New Zealand Association of Oral and Maxillofacial Surgeons
Frequently Asked Questions
An Oral & Maxillofacial Surgeon is a medical and dental specialist who has completed formal advanced training and is recognised as an expert in the field of surgery affecting the teeth, jaws, mouth and face. In addition to both dental and medical university degrees, an Oral & Maxillofacial Surgeon will have undertaken at least six years of additional formal training as well as an extensive assessment and examination process.
An Oral & Maxillofacial surgeon is recognised by the Australian Health Practitioner Regulation Agency (AHPRA) as a specialist in both dentistry and medicine.
It is important to ensure that you see a specialist recognised by AHPRA when you seek specialist treatment.
An Oral and Maxillofacial Surgeon is both a medical and a dental specialist. At Omsspecialists you will see a specialist for consultation and treatment.
Anyone may be seen by a specialist for consultation and treatment. However, to make benefit of any Medicare and private health insurance rebates, specialist consultation and treatments require referral from your GP or dentist. It is therefore important that you bring your referral to your initial consultation, or your referral has been forwarded to Newcastle Oral and Facial Surgery prior to your consultation.
At OMS Specialists, all patients will see a specialist for an initial consultation. During the initial consultation your surgeon will discuss with you, your condition and options of treatment as well as expectations and risks of surgery.
The cost of your consultation may be partly covered by Medicare. It is important that you bring your medicare card with you for your consultation.
As part of your consultation you will also receive a fee estimate of the costs for surgery. If you have health insurance you may be covered either wholly or partly for the costs of surgery. It is important that you discuss with your health fund about your amount of cover once you receive your fee estimate.
- Cost of initial consultation: $195.00; Medicare rebate: $88.25*
- Cost of subsequent consultation: $100.00; Medicare rebate: $44.35*
- Imaging (Cone Beam CT or OPG): $150.00. The cost of imaging may be covered by Medicare if it is part of treatment performed by the OMS Specialists team.
I have health insurance
If you have health insurance, whole or part of your cost may be covered by your insurer. This is dependent of the type of cover you have as well as the type of treatment that is required. If you have hospital cover, your hospital visit or hospital stay may also be covered by your insurer. There are some conditions that are covered under your hospital cover whilst others are only covered by your “extras” or “ancillary cover. It is therefore important to be aware of whether you have hospital cover and any “extras” or “ancillary” cover that might apply to your condition.
I do not have health Insurance
If you do not have health insurance you can “self-fund” your procedure. Should you need a general anaesthetic for your treatment, your total cost will be the cost of the surgery as well as the cost of the hospital and the anaesthetist. We will provide you with details for these on your consultation. Should you need a local anaesthetic for your treatment, the total cost will only include the cost of the surgery. There are however conditions that cannot be treated under a local anaesthetic and will required a general anaesthetic.
* As per the Medicare Benefits Schedule 2020
We aim to provide you with the most efficient and informative consultation process possible. This will allow you and your surgeon make the most of the consultation time together.
In order to do this, please bring with you:
- Referral letter (if you have one)
- Up to date medical history
- Medicare card
- Health Insurance card or policy details
- Relevant xrays or scans
- Relevant blood or other investigation results
For initial consultations please arrive 15 minutes earlier than your schedule time in order to fill the medical and patient questionnaire. Alternatively you can download and pre-fill the form and bring this with you for your consultation.
During your consultation with your surgeon at Omsspecialists you will be advised where your surgery should be performed. The options vary dependent upon the complexity of treatment required and your medical history.
Your treatment will be performed either under a general anaesthetic (asleep) in hospital or under local anaesthetic (awake) at a delegated location chosen by your surgeon. Treatment requiring general anaesthetic may be performed at various hospitals in Port Macquarie, Taree, Newcastle and Hunter region depending on availability and complexity of treatment.
Wisdom teeth (also known as Third Molar Teeth) usually erupt through the gums in the late teens but can erupt at a much later age. They are usually the last teeth to erupt.
Most people have four wisdom teeth, however this can vary between individuals and some can have none. Quite often there is not enough space for the wisdom teeth to erupt, resulting in the tooth becoming “impacted”.The impacted teeth can cause severe problems hence they are recommended to be taken out by an Oral & Maxillofacial Surgeon.
It is usually the lower wisdom teeth that are the cause for problems. However upper wisdom teeth can bite down onto the lower gums. Therefore, both the upper and lower wisdom teeth are usually removed. The removal of wisdom teeth is a common procedure and should be done as soon as possible before any problems get worse.
It is best to remove wisdom teeth whilst a person is young. Young person’s tooth roots have not completely formed and the bone around the teeth is softer. Therefore, removal of wisdom teeth is much easier with fewer complications.
Your Oral & Maxillofacial surgeon may recommend the removal of your wisdom teeth based on the following reasons:
- There is not enough room for the tooth to push through.
- You need orthodontic work and the your orthodontist requires space to align your other teeth by removing the wisdom teeth.
- The tooth has started to cause problems and should be removed before any further damage occurs.
As the wisdom tooth develops, its roots will grow closer to the nerve of the jaw, therefore increasing the risk of injury to the nerve if the tooth were to be removed later.
Protection of adjacent teeth from the impacted wisdom teeth.
There are a variety of conditions affecting the teeth, gums, jaws and soft tissues of the mouth that may require treatment by an Oral & Maxillofacial Surgeon. Surgery in these areas is called dento-alveolar surgery
Some common surgical procedures include:
- Extraction of a tooth or a retained root
- Odontome removal
- Exposure of a tooth
- Freenectomy
- Removal of cysts
- Oral Pathology
- Aid in root canal therapy
- Aid in fitting of a prosthesis
Teeth may require extraction for a variety of reasons. The most common reasons are impacted or misaligned teeth, weakened or diseased teeth, previous failed treatments, as part of orthodontic treatment, extra or supernumery teeth and no longer functional teeth.
Odontomes are primitive or malformed teeth. They can cause delayed eruption or prevent eruption of normal teeth. Occasionally they can also cause infections and swellings.
Exposure of a tooth may be required when it is impacted and has failed to erupt. Exposure of the tooth will help it erupt. Occasionally an orthodontic bracket may be attached to the tooth during the exposure to help it erupt.
A freenectomy is the removal of a piece of soft tissue that attaches either the lip or the tongue to the gums. Occasionally this tissue may prevent full movement of the tongue or affect the alignment of the teeth.
Cysts are fluid filled cavities in the jaws and soft tissues that can occasionally become painful, infected or cause swellings. If large enough they may affect nearby teeth, nerves or strength of the jaws.
Oral pathology refers to any abnormal tissue in the mouth, face or lips. This can vary from something that is slow growing and benign to a potential cancerous lesion. It is important that a specialist reviews you to ensure for the correct diagnosis and treatment.
Root canal therapy refers to the removal of dead nerve and pulp tissue in a tooth. A root canal treatment is performed by your dentist. Occasionally surgery to remove the root tip may be required in conjunction with the root canal treatment.
Comfortable and functional dentures sometimes require removal of hard or soft tissues in the mouth.
If you do not have health insurance you can “self-fund” your procedure.
Should you need a general anaesthetic for your treatment, the total cost will include the cost of the surgery as well as the cost of the hospital and the anaesthetist. We will provide you with details for these on your consultation.
Should you need a local anaesthetic for your treatment, the total cost will only include the cost of the surgery. There are however conditions that cannot be treated under a local anaesthetic and will require a general anaesthetic or IV Sedation.
Other options such as IV Sedation can also save you significant costs.
Your surgeon will discuss this with you.
IV sedation provised a comfortable and calm experience for patients, whether they are highly anxious or unsuitable for extraction under local anaesthetic only. Patients who require extractions, implants or any other minor oral surgery can generally be suitable for IV sedation.

